INTRODUCTION
Secondary cryoglobulinemia is the most common extrahepatic manifestation of hepatitis C (1). There are different genotypes of hepatitis C, and the ones that are most frequently associated with cryoglobulinemia are genotypes 1b and 2a (2). Cryoglobulinemia affects various organs and can cause vasculitis, arthralgia, skin changes, glomerulonephritis and neurological manifestations, including peripheral neuropathy. Cryoglobulins are immunoglobulins that produce precipitate or gel in reduced temperatures. These precipitate dissolve when the temperature returns to normal values (3,4). Cryoglobulinemia can be essential - without a detectable underlying disease, or it can be secondary to other conditions, such as an infection (most commonly hepatitis C) (5), lymphoproliferative or an autoimmune disease. It can lead to a variety of systemic complications, including peripheral neuropathy (3).
The aim of this report was to emphasize the importance of early diagnosis of hepatitis C infection in patients who are presenting with sensorimotor polyneuropathy.
CASE REPORT
Patient information and clinical findings
A 69-year-old woman was admitted to the Department of Neurology in August 2016 due to progressive gait difficulties with distal motor weakness of extremities, tingling sensation in the hands and feet, and skin changes.
The symptoms began in December 2015 after overcoming the flu when the patient developed gradual numbness and weakness of both hands and feet. In February 2016, tests for paraneoplastic syndrome were performed, which came back negative and the patient was diagnosed with polyneuropathy of unknown cause. She was prescribed methylprednisolone in dosage of 4 mg per day that she stopped using of her on own initiative after two months. Several months later, the patient developed new symptoms, now including polyarthritis affecting small joints and both ankles. One month later, due to spinal stenosis that was described on MR imaging, she was referred to spine surgery which resulted in short-term subjective improvement. However, the tingling sensations in both hands and feet persisted, and one month later she developed gait difficulties and now required crutches for walking. Later, in June 2016, the patient developed severe neuropathic pain in distal extremities with skin changes on her ankles. She was then prescribed amitriptyline and pregabalin. In August 2016, the gait got progressively worse with swelling of the joints and prominent skin changes (Figure 1a) due to which the patient was admitted to our Department.
Past medical history revealed arterial hypertension and surgery of the kidney in the childhood that required blood transfusion.
Neurological examination at admission revealed distal motor weakness with hypotrophy, paraesthesia in „stocking – glove“ distribution, absent pain and vibration sensation of the feet, and absent Achilles reflexes, while the physical examination revealed skin ulcerations of the lower extremities.
Diagnostic assessment
Laboratory testing showed elevated sedimentation rate (ESR) and C-reactive protein (CRP) levels, while immunological testing revealed normal ANA; p-ANCA, c-ANCA, anti-CCP anti dsDNA levels, increased RF and CIC, C4 hypocomplementemia and positive cryoglobulin type III. Tumour markers were retested and came back negative, vitamin B12 and folate levels came back within the range.
Electromyoneurography revealed severe, predominantly axonal sensorimotor polyneuropathy.
Neuroradiological imaging (MR of the cervical and lumbar spine), did not reveal any significant findings, and lumbar puncture revealed a slightly increased protein level (0,51 g/L) with normal cell counts (5 cells) and normal CSF glucose levels.
Serologic studies for viral hepatitis were performed and came positive for HCV virus (genotype 1b, 240745 IU RNA/ml). The tests for hepatitis B and HIV were negative.
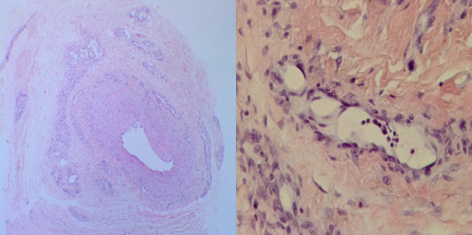
In further investigation, skin biopsy was performed and revealed leukocytoclastic vasculitis with necrosis (Figure 1b).
Therapeutic interventions
The patient was diagnosed with cryoglobulinemia and treated with high doses of glucocorticosteroids during initial hospitalisation (1000 mg for three days following with 500 mg for two days). She was discharged home with prescribed immunosuppressive therapy (prednisone) and antiviral therapy (ombitasvir, paritaprevir and ritonavir + dasubavir) for hepatitis C. On follow-up exams there was a gradual and substantial recovery of skin lesions (Figure 1c), eradication of chronic HCV infection with significant improvement in motor strength (4/5) of the legs.
DISCUSSION
Hepatitis C infection is related to various intrahepatic and extrahepatic manifestations, and cryoglobulinemia is believed to be one of the most common extrahepatic expressions (1,5).
In most cases, cryoglobulinemia is asymptomatic. However, patients who develop symptoms can present with arthralgia, cutaneous changes, vasculitis of various severity, renal and neurological complications (1,2).
Not every HCV infection will be accompanied by cryoglobulinemia and not every genotype of HCV is equally represented. Our patient was diagnosed with type 1b, a genotype that was previously described in studies as one that is most commonly associated with cryoglobulinemia (2).
Furthermore, organ involvement and patient symptoms vary greatly, and not all symptoms are represented equally in every patient. It has been reported that neurological symptoms are more present in patients with type 1b and 3 than in other types (2). However, the reason for this is not yet completely understood (6).
Regarding the neurological manifestations, various authors have reported both central and peripheral neurological complications. Central neurological manifestations were sporadic and included individual cases of seizures, intracerebral haemorrhage, cerebral vasculitis and meningitis (7). More common neurological complications were those of peripheral nerves. These were polyneuropathy, small fibre neuropathy and mononeuritis multiplex (7).
Our patient was asymptomatic for many years. The first manifestation included sensory nerve involvement, followed by polyarthralgia and skin changes. She was later on diagnosed with sensorimotor polyneuropathy, which has been reported as one of the most common neurological complications (6,7).
Available treatment is focused on the underlying disease and includes specific and symptomatic therapy – most commonly corticosteroids, cytostatics, antiviral therapy, plasmapheresis and intravenous immunoglobulin (7). Immunosuppressive or immunomodulatory therapy, including steroids, plasmapheresis and cytotoxic agents, is reserved for organ-threatening manifestations (8). Symptomatic treatment includes treatment of neuropathic pain with pain-modifying agents, including amitriptyline/nortriptyline, duloxetine, gabapentin, or pregabalin and NSAIDs that are used for the treatment of arthritis or arthralgia symptoms (9).
The reported success of the treatment is variable and greatly depends on the time when the therapy was initiated and on the presenting symptoms (2,7,9).Our patient was treated with corticosteroids and antiviral therapy which resulted in recovery of skin lesions, eradication of HCV infection and significant improvement in motor strength, with residual very mild distal motor leg weakness. Despite the long period between the symptoms onset, diagnosis and the treatment, our patient had very good clinical improvement.
In everyday clinical practice, early recognition of cryoglobulinenima and confirmation of hepatitis C infection in patients with sensomotor polyneuropathy may enable early treatment and better functional outcome with reduced possibility of permanent neurological damage.